Home » Posts tagged 'public health'
Tag Archives: public health
Sewage and the Science of Public Health – Dr. Shu-Yuan Cheng and Dr. Marta Concheiro-Guisan Track Wastewater Contaminants

Wastewater is a topic that the average New Yorker doesn’t think about often, but perhaps we should. Sewage and run-off, over a billion gallons of which are treated every single day in New York City by 14 wastewater resource recovery facilities, are a valuable resource for scientists.
Wastewater sampling has been a useful tool for public health researchers tracking the COVID-19 pandemic over the last two years. The Centers for Disease Control (CDC) launched the National Wastewater Surveillance System in September 2020 as a means of tracking virus spread and community prevalence. Viral genetic material is transmitted in fecal matter to the sewers and waste treatment plants, where researchers can take samples. Their work can serve as an early warning of community spread, track variants, and inform public health strategies for responding to the virus. Even better, wastewater surveillance doesn’t require individuals to seek out healthcare in order to capture information, meaning that the resulting data can include people who may be asymptomatic, who have taken home tests, or who have not been tested at all.
Wastewater data have figured prominently in several interesting COVID-19 stories recently in the news. In January 2022 the CDC reported that mutations associated with the Omicron variant showed up in New York City wastewater in November 2021, before the variant was officially reported in South Africa and at least a week before the first U.S. case was identified via clinical testing, suggesting that Omicron was likely circulating in communities before cases could be officially confirmed. And The New York Times recently reported on mysterious fragments of viral RNA with novel mutations detected in NYC wastewater, which are stumping researchers. They haven’t been able to pin down where these fragments are coming from, nor why these mutations have not shown up in clinical testing of human or animal populations in the city.

Two John Jay College researchers, Dr. Shu-Yuan Cheng and Dr. Marta Concheiro-Guisan, are also big proponents of wastewater sampling studies as a public health tool. Their own research, published in 2019, tracked drug use over one year in New York City, using one-time grab samples to test for levels of cocaine, nicotine, cannabis, opioids, and amphetamines in the sewage. Now, the scientists are collaborating with non-profits that test the health of the city’s waterways, trying to correlate levels of pharmaceuticals in our rivers with the amount of harmful bacteria.
To Dr. Cheng and Dr. Concheiro-Guisan, wastewater analysis’s great strength lies in early warning and early intervention. “It’s a great tool for prediction, for public health, crime fighting, and disease [prevention] purposes,” says Dr. Cheng. “The official report is often too late, but if you can do an early intervention, find the issue and start addressing it, there’s a lot you can do.”
“We looked at wastewater because we saw the utility,” says Dr. Concheiro-Guisan. “This is a different application [than viral tracking] but with the same thought: that what we eliminate from our bodies tells you a lot about your population.”
However, the United States is late to the game. Though the CDC has had results with its national COVID-19 tracking program, both researchers lament the lack of a centralized American body to apply this research to other public health applications. They’d like to see the U.S. follow the example set in European countries, China, Australia, and increasingly in South America, where governments have applied wastewater sampling to create campaigns warning their citizens about novel psychoactives, catch drug manufacturers, and more.
“It’s a very important public health tool that is showing results,” says Dr. Concheiro-Guisan. “If you start in the biggest city in the country, if you start in New York, then others will follow.”
 Dr. Shu-Yuan Cheng is an Associate Professor and Chair of John Jay’s Department of Sciences. Her research is in the areas of toxicology and forensic pharmacology, including the roles that environmental toxins play in neurodegenerative diseases, identifying the target genes and signaling pathways affected by environmental toxins, and investigating pharmacological mechanisms of anti-cancer medications.
Dr. Shu-Yuan Cheng is an Associate Professor and Chair of John Jay’s Department of Sciences. Her research is in the areas of toxicology and forensic pharmacology, including the roles that environmental toxins play in neurodegenerative diseases, identifying the target genes and signaling pathways affected by environmental toxins, and investigating pharmacological mechanisms of anti-cancer medications.
 Dr. Marta Concheiro-Guisan is Assistant Professor of Forensic Toxicology in John Jay’s Department of Sciences. Her research focuses on the development and validation of analytical methods by gas and liquid chromatography tandem mass spectrometry and their application to different specimens, the detection of drug exposure during pregnancy, and the toxicological study of new psychoactive substances.
Dr. Marta Concheiro-Guisan is Assistant Professor of Forensic Toxicology in John Jay’s Department of Sciences. Her research focuses on the development and validation of analytical methods by gas and liquid chromatography tandem mass spectrometry and their application to different specimens, the detection of drug exposure during pregnancy, and the toxicological study of new psychoactive substances.
Gerald Markowitz shines light on corporate bad behavior
Distinguished Professor of History Gerald Markowitz and long-time writing partner David Rosner, a Professor of Sociomedical Sciences at Columbia University, have been researching industrial pollution and contaminants since the early 1970s. Their first jointly-authored book, Deadly Dust: Silicosis and the Politics of Occupational Disease in Twentieth-Century America, explored historical evidence of the lung disease silicosis, which is a hardening of the lungs due to inhaling dust found in sand or rock. Thanks to Deadly Dust, Markowitz and Rosner came to the attention of lawyers bringing workplace safety suits on behalf of construction workers suffering from silicosis, launching a long career of research and expert testimony on occupational disease and toxic substances. In the early 2010s, the duo began an investigation into asbestos and asbestos-related disease.
 Their work turned up hundreds of articles on the dangers of asbestos, now a watchword for poisons that can lurk in our homes, dating from 1898 to the present. Markowitz and Rosner also referred to corporate records and documents made public through court discovery; a more recent project called ToxicDocs is an open-source, online database of more than 15 million pages of documents related to silica, lead, vinyl chloride, and asbestos that were previously not easily accessible.
Their work turned up hundreds of articles on the dangers of asbestos, now a watchword for poisons that can lurk in our homes, dating from 1898 to the present. Markowitz and Rosner also referred to corporate records and documents made public through court discovery; a more recent project called ToxicDocs is an open-source, online database of more than 15 million pages of documents related to silica, lead, vinyl chloride, and asbestos that were previously not easily accessible.
In June, Markowitz’s expertise was featured prominently in the American Journal of Public Health, in an article detailing a representative episode in the history of the struggle between industry and regulators. In “Nondetected: The Politics of Measurement of Asbestos in Talc, 1971-1976,” Markowitz and his co-authors describe the years-long interval between the talc industry’s acknowledgement that asbestos is toxic and their taking action to protect consumers, and the subsequent conflict between the Conflict, Toiletry, and Fragrance Association (CTFA) and the U.S. Food and Drug Administration (FDA) over regulating appropriate methods for detecting asbestos contamination in consumer talc products and setting safety standards.
The focus of the article, said Professor Markowitz, “was that the cosmetic industry, I think very consciously, used this concept of nondetected, which we as consumers think of as ‘no asbestos in the talc,’ but nondetected could mean enough asbestos in the talc to cause disease. And that’s what the industry understood, but consumers did not.”
The CTFA’s 1970s victory in lowering detection standards and advocating for self-regulation is still bearing fruit; recent lawsuits against talcum powder manufacturers allege the household product causes cancer due to asbestos contamination. As recently as 2018, courts awarded plaintiffs record damages of close to $4.7 billion in a case against manufacturers, capturing public attention.
We sat down with Professor Markowitz to talk about his work researching industrial poisons and about corporate responsibility to the consumer in today’s world. Read on to hear from Professor Gerald Markowitz in his own words.
Why do you believe that talc product manufacturers continued to accept a lower standard for asbestos eradication despite known health dangers, not to mention the risks of litigation?
When they developed this idea, in the 1970s, their basic argument was that there should be as little federal regulation as possible. [The CTFA] was able to lobby the federal FDA that the technologies that the FDA was proposing were not able to be completely accurate, would give too many false positives, would take a long time to do, and would be costly. So they proposed their own method. And they’re able to eventually convince the FDA that it should not be federal but industry regulation.
But what they admit privately is that their method, which is not as demanding as the FDA’s proposed method, was not necessarily accurate and was not necessarily consistent. So to a certain extent, they were really able to forestall regulation by claiming that they could do as good a job [of detecting asbestos in talc products], even though they themselves admitted that they could not do as good a job. And by the very nature of their method, they were going to uncover much less asbestos than the FDA’s method was capable of uncovering.
Do you think there’s something special about the current moment that made this article of particular relevance?
I think it was the variety of ways that deregulation has had an impact on the health and welfare of people in the United States and other parts of the world. To the extent that these articles could help to call attention to that happening, they are important. The advantage of history is that we are able to really see the process unfold in a kind of detail that we don’t necessarily have in observing regulatory of anti-regulatory actions taking place at the moment we’re living in. That level of detail I think is instructive in terms of being able to understand how similar things could be happening today.
Would you like to see this history galvanize some kind of action?
The most important thing that can happen is that people really have to take politics seriously. The United States has a long history of mass movements really demanding and achieving fundamental reforms. Just going back to the 1960s, the demand for civil rights, the efforts of people to get voting rights for African Americans, that didn’t happen simply because Congress decided to pass a law; people were demanding it in mass actions. These are really instructive in terms of what can happen today, and even what is happening today.
Pieces accompanying your article in the AJPH, such as the one by former Assistant Secretary of Labor for the Occupational Safety and Health Administration David Michaels, suggest that corporate influence is getting stronger, to the detriment of consumer and public health. The current administration has loosened or degraded regulatory standards for a variety of products — should we expect more legal battles down the line?
Yes, absolutely. Since the 1970s there has been a very sustained effort by many businesses to oppose regulation, and you get the classic statement by Ronald Reagan, when he said that ‘government isn’t the solution, government is the problem.’ I think the legacy of that, of the push for deregulation as a means of stimulating the economy and freeing business to innovate and all of those kinds of ideas, I think the legacy of that is going to be a variety of problems, not only in consumer products but in environmental damage. It’s going to be for workers, for consumers, for people living in communities where toxic substances are going to be released, we’re going to be suffering those consequences, and the unfortunate thing is that it’s only going to be remedied in retrospect.
And to add one other element, we know that the burden, especially of environmental pollution, toxic waste, global warming, is going to affect poor communities and communities of color to a much great extent than richer communities. At a college emphasizing social justice, this becomes an even more vital issue.
Are there other consumer products known to include dangerous adulterants that are similarly being ‘underregulated?’
BPA [bisphenol A, a chemical used to make certain plastics since the 1960s] is one example; a lot of household cleaners and flame retardants are another one. We’ve discovered that flame retardants are extremely dangerous to people, and that people have them in their bodies. Formaldehyde is another one; there was a scandal about formaldehyde in temporary housing given to people after Katrina, that was unsafe.
There are lots of things we have clues about, but the real scandal is that chemicals are being produced and we’re using them in very large quantities, that have never been tested. And in the United States we have this philosophy, innocent until proven guilty. It’s the same philosophy with chemicals — they are innocent until proven guilty. The Europeans have a system, chemicals can’t be introduced until they’re proven safe. It’s a basic difference in philosophy that companies need to prove that something is safe before they can experiment on us and ensure it doesn’t cause cancer. But in the United States they say that if it does cause cancer, we’ll take it off the market, but that’s very difficult to prove and you’ve done the damage already.
You note in your article that talc researchers were disappointed when their work became known to the industry, but that ‘nothing was done until the results became public.’ Do you think it remains true in cases of corporate wrongdoing that nothing is done until the public finds out all the information?
In the 1970s, there was this wonderful act passed called the Freedom of Information Act (FOIA). The fundamental principle behind that was that if you shine the light of publicity and information and people have that, then they have the ability to act in their own interests. One contribution that historians can make is, using the older historical records, we can cast a light on activities and attitudes and actions that permit people to see what is going on and demand change.
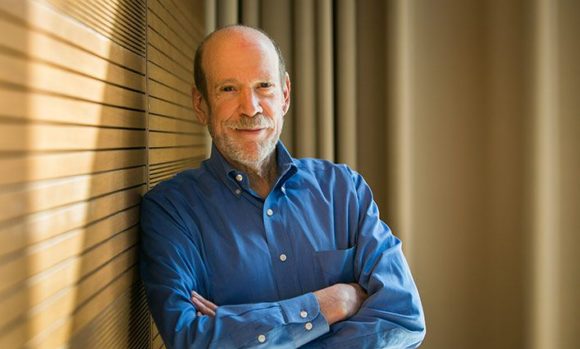
Gerald Markowitz is a Distinguished Professor of History in the Interdisciplinary Studies Department at John Jay College and the Graduate Center of CUNY. His research focuses on the history of public health in the 20th century, environmental health, and occupational safety and health. He has authored a number of books, most recently Lead Wars: The Politics of Science and the Fate of America’s Children, also in cooperation with David Rosner.
John Jay Scholars on the News – Vaccines and the Flu
It’s winter, which we sometimes call “flu season.” In fact, “you can catch influenza at any time during the year if exposed to the virus, and its severity is the same regardless of when you get sick,” says Edgardo Sanabria-Valentín. We don’t fully know the answer to why influenza is more common during the colder months. According to Nathan Lents, “The virus is viable for a longer time in cold air, and spreads more readily in dry air. Another reason that may contribute is that winter air dries our mucus membranes, which makes them less effective at preventing viral entry. We also tend to spend more time indoors with closed windows and recirculated air.”
A somber anniversary

The 2018 flu season was also the 100th anniversary of the infamous global influenza pandemic, a year when more
than 500 million people around the world are estimated to have died from flu. Of that number, 675,000 fatalities came from the United States, with roughly 20,000 from New York City alone. According to Mike Wallace, in his 2018 book Greater Gotham, more Gothamites died of disease in the city than died during World War I; the ongoing war effort actually impaired New York’s efforts to fight the flu, by concentrating soldiers in training camps where disease could spread and by taking much-needed medical personnel away from home to establish medical camps near the battlefields in Europe.
Despite the high numbers of fatalities at home, New York of 1918 had a lower death rate than other major cities (4.7 deaths per 1,000 residents, as compared to Boston’s rate of 6.5 and Philadelphia’s of 7.3). This was attributed by Health Commissioner Royal Copeland to New York’s long history of public health work, and particularly the alleviation of unhealthy conditions around the city at the turn of the 20th century.
Vaccines and you

Today, scientific and public health efforts have brought some protection from a repeat of 1918 in the form of vaccines. In the case of the flu, explains Dr. Lents, “Each year’s vaccine is targeted toward the three to four strains that appear to be spreading the most rapidly. The injected vaccine contains killed viruses [from those strains], while the nasal spray contains live but weakened viruses. In both cases, the large dose of viral particles elicits a strong immune reaction from our bodies, including the production of antibodies that can stick around for years or even decades. The second time we are exposed to the same virus, it only takes a day or two to mount the same level of immune response. This ‘priming’ gives the immune system enough of a head start that it usually prevents the infection from ever taking hold.”
Because the influenza virus is so good at mutating from year to year, “no vaccine is 100% perfect, and getting the flu shot will never protect you against 100% of all flu strains,” says Dr. Sanabria-Valentín. But the vaccine will “significantly decrease the risk of getting sick, and will decrease the severity and length of infection, and decrease the chance that you get other people sick” if you do contract the virus.
Vaccinating also helps to protect those around you in other ways, namely by contributing to “herd immunity.” “Some people cannot be vaccinated because they are too young, too old, immune-compromised, or battling other kinds of infections,” says Dr. Lents. When the percentage of people in a population are effectively immunized, it helps to prevent the spread of disease to those who were unable to receive the vaccine. But when the percentage of vaccinated people falls because individuals who otherwise could be immunized choose not to be, it puts vulnerable populations at risk.
Conquering vaccine hesitancy

“Controversies about vaccinations have been out there since we adopted this preventative measure almost 100 years ago,” says Dr. Sanabria-Valentín. “There are a lot of myths about vaccinations which are peddled by conspiracy theorists trying to sell you something or by people who might have good intentions but got swindled by ill-intentioned people trying to make a fast buck. One of the most popular ones is that vaccines can cause autism in children. This claim was first made in a study that was demonstrated (by many groups) to be fraudulent; no direct relationship between receiving vaccinations and autism has been found. There is overwhelming consensus among scientists and physicians that vaccines are safe and effective even though, like most medical treatments, in very rare cases they can cause side effects and in even rarer instances can cause serious unintended health problems. There is overwhelming evidence that vaccination has helped not just individuals, but humankind.” Although diseases like smallpox, polio and the measles were all but eliminated by vaccine technology, skepticism about immunization–which many attribute to the rise of social media–has caused some long-gone diseases to stage a comeback.
Dr. Lents stated that “in 2017, 80,000 people died of influenza, the highest number in 40 years. If more healthy people had been vaccinated, that number could have been much less. Each person that decides not to vaccinate adds a little bit of risk to the entire population.” This dynamic played out in October 2018, when measles–which was declared eliminated in the US in 2000–broke out in Williamsburg, Brooklyn. The New York City Department of Health confirmed 42 cases in Williamsburg and Bensonhurst as of mid-December, and is currently barring un-immunized students from attending local schools. And according to The Guardian, Europe is also experiencing a surge in vaccine hesitancy and a corresponding growth in the numbers of new measles cases; Europe will see more than 60,000 new cases this year and 72 deaths, the highest number this century.

It is generally agreed that fears about vaccine side-effects are overblown, and contradicted by scientific consensus. “Vaccines are constantly monitored and modified as circumstances dictate. The FDA does not approve a vaccine unless initial trials indicate the benefits clearly outweigh the risks. In response to vaccine safety concerns today, healthcare providers have to give vaccine information sheets to recipients clearly describing the risks and benefits of the vaccine. And finally, vaccines are subject to particularly high safety standards because, unlike other health treatments, they are given as preventive measures to protect healthy people,” explains Dr. Evelyn Aranda Jaque. “Although vaccination is not 100% effective, studies on flu vaccination programs have shown that people who get vaccinated are less likely to be seriously ill or die in comparison with those who do not vaccinate. We must consider that the widespread use of vaccines for life-threatening diseases in the United States has led to a dramatic decrease in their incidence.”
Evelyn Aranda Jaque is a substitute Associate Professor at John Jay College, where she teaches classes including Immunology and Microbiology. She received her Ph.D. from the Physiology Department at Pontificia Universidad Católica de Chile. Dr. Aranda Jaque’s research since her doctorate days has largely focused on the role of angiogenesis (the formation of new blood vessels) in tumor progression.
Nathan Lents is a Professor of Biology and Director of the Honors Program and Macaulay Honors College at John Jay College. He holds a Ph.D. in human physiology and postdoctoral training in computational biology from NYU. In addition to his laboratory research, Dr. Lents writes popular science articles, blog and books. His most recent book is Human Errors: A Panorama of Our Glitches from Pointless Bones to Broken Genes.
Edgardo Sanabria-Valentín is the Associate Program Director of John Jay College’s Program for Research Initiatives in Science and Math (PRISM) as well as the college’s Pre-Health Careers Advisor. He holds a Ph.D. from NYU-School of Medicine, and spent three years working in the biotechnology industry. Dr. Sanabria-Valentín is the recipient of the ESCMID Young Scientist Award (2007), a Leadership-Alliance Schering Plough Graduate Fellowship (2006), and the NBHS-Frank G. Brooks Award for Excellence in Student Research (2001).
Mike Wallace is a Distinguished Professor of History at John Jay College and author of Greater Gotham: A History of New York City from 1898 to 1919. Dr. Wallace is also the co-author of Pulitzer Prize-winning Gotham: A History of New York City to 1898 and the founder of the Gotham Center for New York City History at the CUNY Graduate School. He received his undergraduate and graduate degrees from Columbia University.
John Jay Scholars on the News – The Opioid Epidemic
The terms “opioid crisis” or “opioid epidemic” have come to be used as political buzzwords, but what does it really mean to say that America is in the grip of an “opioid epidemic”? According to the Centers for Disease Control, more than 72,000 people in the United States died as the result of an overdose in 2017, and approximately 30,000 of these were from the use of fentanyl and other synthetic opioids — that comes to around 100 per day! Fentanyl, a powerful opioid designed to treat severe and chronic pain, is roughly 100 times stronger than morphine, and is currently being used to adulterate other abused substances, making these overdoses likely to increase.
From the perspectives of policy, policing, and public health, this rash of deaths is worthy of further consideration. John Jay College scholars from across disciplines and research areas tell us what they think has contributed to the trend of deaths from opioid abuse and what approaches may be best suited to tackling the problem.

What is different about the pattern of drug abuse we are seeing today that has caused it to be referred to as the “opioid epidemic”?
Jeff Coots (Director, From Punishment to Public Health Initiative): One main reason for concern around opioids today is that they are simply more deadly than the other drugs we consume. However, the rates of overall illicit drug use are actually quite steady — especially when we remove cannabis consumption from the conversation. The latest results from the National Survey on Drug Use and Health show steady illicit drug consumption from 2002-2013 at about 4%, with those aged 18-25 using a bit more than twice the rate of other age groups. We do see a slight increase in heroin consumption as prescription opioids become less available, but this doesn’t impact the overall rates of illicit consumption.
Heidi Hoefinger (Visiting Scholar, Anthropology): The situation is considered an “opioid epidemic” due to the size of the problem now, and its potential for growth. But this issue is also getting more attention than past drug “epidemics” because it’s a white, middle-class problem, particularly here in New York, with Staten Island and Long Island having some of the highest rates of use and overdose. There has definitely been a “softer” approach to this epidemic as opposed to the “crack epidemic” of the 1980s, which saw much more aggressive law and order efforts resulting in mass incarceration. Many poor people of color are still sitting in prison because of that heavy-handed approach. It’s definitely a good thing that opioid addiction is currently being viewed as more of a public health issue, but it’s extremely problematic that Black and Latinx folks continue to suffer the consequences of racist applications of drug policy.
Can you point to a few of the key factors that you believe are to blame for the current public health crisis?
Jeff: The origins of the current crisis began with the marketing of OxyContin as a non-addictive painkiller in the 1990s followed by the introduction of “pain” as the fifth vital sign in 2001. This led to higher rates of opioid prescription drug use and related overdose fatalities in the early 2000s. The second “wave” of opioid-related deaths are attributed to increased heroin consumption starting in about 2010, following a crackdown on prescription opioid distribution — consumers simply switched to the cheaper and more available opioid. The third wave is attributed to the increased presence of synthetic opioids like fentanyl in the market, starting in about 2013. These synthetics can be much more potent and make it difficult for users to control their dosage, leading to more overdoses.
Marta Concheiro-Guisan (Assistant Professor, Forensic Toxicology): Other socioeconomic factors like unemployment and economically-depressed areas should also be considered in trying to understand the whole problem and the populations most affected by it.
Heidi: The biggest drivers are probably Big Pharma and corporate greed because pharmaceutical companies were deceptive about the true effects of opioids, claiming they were non-habit inducing. They also offered incentives to doctors for prescribing, which led doctors to over-prescribe opioids instead of safer alternatives. Insurance companies typically cover opioids as opposed to alternative therapies, so they’ve played a role in this as well. It’s encouraging to see that NYC (among other cities) is suing some major pharmaceutical companies for their role in the epidemic, but there still needs to be more accountability on the part of Big Pharma.
What are the implications for American society should this systemic issue continue unabated?
Jeff: I think we are having a really important debate in the country right now about how our collective response to drug use differs along racial lines. Drug Policy Alliance and Columbia University co-hosted a conference in 2016 to highlight how the white opioid user who may have started on prescription drugs and then switched to heroin is considered a victim of circumstance and provided overdose treatment, rehabilitation and a call for compassionate public health responses. Meanwhile, black and brown heroin addicts who may not have had health insurance and access to prescription drugs tend to get jail cells, court-mandated treatment and moralizing “just say no” campaigns grounded in personal responsibility. Obviously, the the shift towards funding treatment and reducing criminal justice involvement is welcome, but the carnage reaped in the previous regime of zero tolerance and deterrence must be acknowledged and reconciled at the local and national levels.
Heidi: It has been compared to HIV in some arenas, in that it’s affecting a marginalized and stigmatized population (e.g., drug users) but it’s not getting the same attention and funding it deserves. The numbers of overdoses and deaths will likely continue to rise as long as the stigma exists, and as long as pharmaceutical companies continue to operate unchecked, as long as doctors continue over-prescribing, as long as insurance companies don’t see the value in covering alternative treatments, and as long as harm reduction remains undervalued and underfunded.
Marta: The biggest impact on American society is, of course, the tragedy of the families affected by this unprecedented health issue, and the loss of so many young people’s lives. The Centers for Disease Control and Prevention estimates that the total “economic burden” of current opioid misuse alone in the United States is $78.5 billion per year, including the costs of healthcare, lost productivity, addiction treatment, and criminal justice involvement.
 The Opioid Crisis Response Act of 2018 was recently signed into law. It authorizes new funding and grants to address the crisis, advances initiatives to raise awareness and to get more first responders to carry naloxone, and drives increased coordination among federal agencies to stop drugs like fentanyl at the border, among other measures. Do you think this bill takes the right approach to dealing with the crisis? Does it go far enough?
The Opioid Crisis Response Act of 2018 was recently signed into law. It authorizes new funding and grants to address the crisis, advances initiatives to raise awareness and to get more first responders to carry naloxone, and drives increased coordination among federal agencies to stop drugs like fentanyl at the border, among other measures. Do you think this bill takes the right approach to dealing with the crisis? Does it go far enough?
Heidi: Many of these are welcome changes, and are actually similar to Obama’s opioid plan from 2016, but the problem is that this plan doesn’t allocate much more funding — which is needed. If this is a serious public health problem, it should receive funding and attention similar to that provided for HIV/AIDS or Ebola, as well as a similarly concerted, multi-organizational response. But addiction is still a very stigmatized condition, and not taken as seriously as it should be. People with addictions are still often blamed for their own demise, and not viewed in the same light as people with other chronic illnesses.
Marta: From my point of view, one critical element in addressing this crisis is the treatment of addiction as a health issue rather than as a stigma, and a drastic improvement of current services and their accessibility. Another important aspect is education for the general population and among professionals such as medical doctors. More funds are also necessary for the forensic sciences to develop a clearer picture of the current crisis, to know all the opioids that are involved, to monitor future crises, and to research addiction.
Jeff: We need to invest heavily in reducing demand and mitigating the risks associated with consumption, rather than focus on interrupting supply. Efforts to control access to drugs have failed for over a century. In reducing demand, we need to do a better job of addressing pain and trauma, take a hard look at our overreliance on pharmaceuticals and reduce the number of people who become addicted in the first place. In working with those already experiencing opioid dependence, we need to provide competent and evidence-based care including Medication Assisted Treatment (MAT), which is the gold standard for treating those with opioid disorders. In terms of mitigating risks, increased naloxone access is crucial, but increased use of other Harm Reduction strategies is needed as well.
What do you believe is the best way to address this epidemic?
Marta: This epidemic has to be addressed with a multidisciplinary approach, as indicated by the National Institute on Drug Abuse (NIDA) and other governmental agencies. Promoting the use of naloxone, the improvement in the accessibility of medical assistance and addiction treatments, the expansion of prevention programs in schools and for the general public, and increasing funds for the forensic sciences and addiction research are among what I consider the priority areas.
Jeff: The best way to reduce the impact of opioid overdose fatalities is to focus on saving the lives of those who choose to consume opioids. This strategy, more commonly known as Harm Reduction, focuses on reducing the negative side effects associated with illicit drug use, rather than punishing and/or moralizing at those who engage in use. These strategies include needle exchange programs, peer-based education, MAT programs, and safe consumption facilities, all of which treat those who consume illicit drugs as human beings worthy of compassion and competent medical care for their medical issues. As I noted earlier, our previous strategy of interrupting supply and punishing consumption — i.e., the War on Drugs — has not reduced the rates at which our citizens consume illicit drugs. It has, however, made that consumption more dangerous and more damaging for those communities with higher rates of use and criminal justice presence.
Heidi: Societal attitudes towards drug users and people with addictions need to change. For this to happen, people need to understand that drug use has always been a part of human history, drug users are not inherently bad people, and people will continue to want to alter their consciousness or treat pain through drug use. People also need to understand the racialized history of drug policy in this country, and that laws against drug use (which are unevenly applied across race and class) were implemented for racial, class and economic reasons (and because of who was using the drugs), not necessarily because of the harmful effects of the drugs. When people are exposed to this history, and these realities, then perhaps stigma against drug use will change, and people affected by the current epidemic will get the proper help that they need.
In addition, we need more funding for harm reduction and evidence-based drug education programs in middle schools, high schools, college and universities. Not the “Just Say No” type, because those don’t work. But the kind where students can ask open, honest questions and get factual, evidence-based, non-biased, non-moralistic responses so they can know the potential effects and risks and make more informed decisions. And there also needs to be more support for medication-assisted treatment programs (like methadone and buprenorphine), as well as harm reduction programs like DanceSafeNYC that provides factual, evidence-based drug education and drug checking kits at music festivals and events. These types of initiatives take harm reduction beyond syringe exchange programs and make them more accessible to a diverse range of young people, which ultimately saves lives, and may start to turn the tide of this epidemic.

Marta Concheiro-Guisan, Ph.D., is Assistant Professor of Forensic Toxicology at John Jay College. She has experience in the development and validation of new analytical methods and toxicological analysis of different types of specimens–including plasma, blood, urine, oral fluid, hair, sweat and other tissues. She has participated in Drugs and Driving Research Projects, including the ROSITA (Road Site Testing Assessment) and DRUID (Driving Under the Influence of Drugs) European Projects, to study alternative matrices to detect drug impairment, and in clinical protocols involving different types of drugs of abuse and drug exposure during pregnancy. Dr. Concheiro-Guisan has more than 40 publications in peer-reviewed journals.
 Jeff Coots, JD, MPH, serves as the Director of the From Punishment to Public Health (P2PH) initiative based at John Jay College. Prior to joining P2PH, Mr. Coots completed a joint Juris Doctor/Masters of Public Health degree program at Northeastern University School of Law and Tufts University School of Medicine, where he focused his studies on the social justice and health impacts of mass incarceration. While in Boston, he served as an Albert Schweitzer Fellow and delivered dialogue-based “Health Reentry” workshops to introduce strategies for working in collaboration with a primary care provider to prevent new infections and mitigate the effects of chronic disease.
Jeff Coots, JD, MPH, serves as the Director of the From Punishment to Public Health (P2PH) initiative based at John Jay College. Prior to joining P2PH, Mr. Coots completed a joint Juris Doctor/Masters of Public Health degree program at Northeastern University School of Law and Tufts University School of Medicine, where he focused his studies on the social justice and health impacts of mass incarceration. While in Boston, he served as an Albert Schweitzer Fellow and delivered dialogue-based “Health Reentry” workshops to introduce strategies for working in collaboration with a primary care provider to prevent new infections and mitigate the effects of chronic disease.
 Heidi Hoefinger, Ph.D., is a Visiting Scholar in John Jay College’s anthropology department, where she teaches a course on gender and sexuality within the social and cultural contexts that exist in an increasingly integrated but unequal global world. She also works on a large European Research Council (ERC) project led by Kingston University in London, in which she is the New York-based ethnographer looking at anti-trafficking efforts in New York City, and their effect on sex work/ers and migration policy. Among her areas of interdisciplinary research interest are gender and sexuality, globalism and transnationalism, and drug use.
Heidi Hoefinger, Ph.D., is a Visiting Scholar in John Jay College’s anthropology department, where she teaches a course on gender and sexuality within the social and cultural contexts that exist in an increasingly integrated but unequal global world. She also works on a large European Research Council (ERC) project led by Kingston University in London, in which she is the New York-based ethnographer looking at anti-trafficking efforts in New York City, and their effect on sex work/ers and migration policy. Among her areas of interdisciplinary research interest are gender and sexuality, globalism and transnationalism, and drug use.
National Network for Safe Communities Hosts Film Screening, Panel on Opioid Crisis
By Raymond Legendre
Amidst the deadliest drug epidemic in American history, the National Network for Safe Communities (NNSC) hosted a documentary film screening and panel discussion on October 2 that highlighted why the opioid crisis is so difficult to stop, and shared the actions being taken in New York City to save lives.
The event featured the Mother Jones short documentary series, Finding a Fix, with a brief introduction by filmmaker Mark Helenowski, and a subsequent panel conversation including New York City council member Stephen Levin, Manhattan Assistant District Attorney Kaitrin Roberts, and community organizer Marilyn Reyes, co-chair of the Peer Network of New York. Mother Jones reporter Julia Lurie also participated on the panel, which was moderated by NNSC Director David Kennedy.

In 2017, drug overdoses claimed an estimated 72,000 lives in the U.S., according to the Centers for Disease Control and Prevention. Of those deaths, more than 49,000 were attributed to opioids. New York City alone recorded around 1,500 overdose deaths last year. The current death rate is equal to one New Yorker dying from an overdose every six hours, according to ADA Roberts. The availability of Narcan, a nasal spray that can reverse opioid overdose, is often the different between fatal and non-fatal overdoses, the prosecutor also noted. In August 2017, New York became the first state to make no-cost or lower-cost medicine to reverse opioid overdoses available at pharmacies.
To learn more about the event, read the rest of this article on the NNSC website. To learn more about the work NNSC does, visit their homepage.



Recent Comments